I waited for twenty years to hear that phrase. I blogged in the past about an eating problem I’ve had since college. Last fall it was “solved.” I didn’t write about it because I was playing the long game to see how the medication worked, whether I could get the photos from the surgeon, and so on.
The first time I remember having the problem was during Christmas dinner at my parents’ house. Of course, holiday dinners were a regular occurrence before I moved to California, so it’s unclear what year this happened other than “college.” It’s highly likely that we were eating cornish hens, as that became a Long household staple around the holidays since none of us really liked turkey as much as we were supposed to. I probably thought that first time it happened that I had just choked on a hen bone or something.
Turned out it was the “or something,” but it would take twenty years to find out what.
Flash forward to 2006 and this had become a regularly occurring random problem in my life. I would be eating and a bite just wouldn’t go down, stuck in my throat, often requiring me to expel in the restroom. This happened at home, while walking down the street, in foreign countries, with coworkers, with friends, with family. It was a constant threat and source of anxiety around an experience that for everyone else is one of the great joys of being a living human being. An inconvenience at home, but an embarrassment elsewhere. Moreover, when out with Sam, there’s an extra dose of guilt for leaving her alone at the table.
After this happened at a restaurant with friends in 2006 (detailed in the previously linked post), I went to urgent care. No help there. After barium tests and x-rays, I was informed there was nothing wrong with me. This began another twelve years of amateur doctors among my peers informing me that it was “all in my head” and/or I “just need to drink some water.”
Having existing anxiety issues only made this situation worse, but nothing I tried seemed to make a difference. It would happen when I was relaxed at home watching a movie enjoying dinner on the couch.
That’s not entirely true that nothing made a difference. I noticed that it never seemed to happen when eating liquids (soup, yogurt, etc.), and tended to show up when eating drier sharper foods (white meat, raw carrots, raw broccoli, etc.). This began an obsession with sauces and mixing my food together, which brought other unintended health complications. Dump ranch on everything and you might not have to cough it up, but it’s also going to stick around longer on your waist.
This trained my gut bacteria to crave fats, oils, and sugars. Condiments became the meal. Pizza needed to be greasy and dipped in ranch (and I’m not just talking about the crust, I dipped every bite!). A funny affectation to friends and family, but a secret tool to stave off embarrassment for me that evolved into an unhealthy craving.

Flash forward to April 2012. On a visit to Zion National Park with my parents and Sam, we decided to get a beer sampler at Zion Pizza and Noodle Company. I didn’t have to cough anything up, but back at the hotel, my esophagus started painful spasms that lasted for hours.
At this stage of my life, I’d never been a beer drinker. The extent of my alcohol experimentation stopped at wine coolers in college and the occasional celebratory prosecco in adulthood.
In 2014 I joined a weekly hiking group. We brought different types of food and drink to feast at the end of the multiple-mile vertical climb. When you’re exhausted and dehydrated, cold lager is the best thing you’ve ever tasted.
I suspected that an ingredient in beer caused the spasms at Zion, and sometimes I’d experience the same condition after the hikes. Since alcoholic drinks do not have ingredients lists, it was difficult to identify the trigger. Plus, in statistical terms, I was performing multivariate testing on these hikes without a control, obfuscating the effects of any one segment. In lay terms: were the spasms that night the result of the can of Coors Light, the glass of merlot, the cup of soju, or the shot of whiskey? Hard to follow an elimination diet when folks keep bringing you new tastes to try every week!
NOTE: we learned each others’ individual tolerance levels and kept folks in check to make sure all drivers were not a danger to themselves or others at the end of the night. A single wine bottle might be divided among ten hikers, nobody was getting “wasted.”
That fall, a friend asked Sam and me to try BlueApron and write about it for her (now defunct) fitness blog. One of the dishes we made replaced rice with barley.
As soon as I took the first spoonful of the barley the esophageal spasms began. Barley. Beer is made with Barley! The stronger the barley content, the stronger the reaction. The more I looked into it the more this made sense. When I drank lagers that relied more on rice (cheap stuff like Coors light) I didn’t have a strong reaction. Pull out an IPA and… get ready for the hurt.
So that was step one in 2014: I have a barley allergy. This was a new one for a guy that has struggled with managing allergies of varying severity for three decades, but it wasn’t over yet.
Even after cutting out barley, food still got stuck in my throat. It was as if the two were unrelated problems occurring in the same organ, like someone suffering from pink eye and cataracts at the same time and expecting antibiotics to fix everything.
Flash forward again to 2018. I came down with a cold and looked for Nyquil before bed. We’d just remodeled a few months earlier; part of living through a remodel is throwing out absolutely everything you don’t need. For Sam, that included the entire medicine box. All I could find that night was a Nyquil horse pill I’d bought on a work trip a year and never removed from my laptop bag.
The pill wouldn’t go down. It got stuck like so many pieces of food had for two decades. But this wasn’t barley or overcooked steak, this wasn’t even food at all. This wasn’t an allergy. I’d taken pills my entire life and never had this problem. The klaxon in my mind started blaring. While googling “esophegeal cancer symptoms” I emailed my doctor for a gastroenterology referral in order to schedule an endoscopy.
About two weeks later I was laying in a pre-op bed with an IV drip waiting to get wheeled in. Once in the surgical room, the gastroenterologist asked me a few questions and said he probably knew exactly what was going on.
An hour later I woke up in recovery and was told that they’d found many (not sure how many) strictures in my esophagus and they’d stretched them out with a “boogie.” Yeah, I know, sounds like booger. Get over it. They pushed an expandable rubber booger through my throat to stretch out the strictures via esophageal dilation.

So what’s a stricture? Scar tissue. So much built up over time that it forms visible rings in the esophagus. In my case they weren’t just visible, they were debilitating, closing off my esophagus to the size of a pea in spots.
No wonder food got caught. It wasn’t nerves or lack of water, my esophagus couldn’t squeeze via peristalsis food through the tiny hole. Thus why soup and liquids didn’t cause problems, they just fell through because of gravity. A sticky piece of white meat could just block it, and swallowing more food (or water) would just pile more on top, potentially making it worse.
Even though my throat hurt and I had to eat yogurt for a day after the operation, I was elated. I knew what was going on in my body for the first time.
And I knew what it was called: Eosinophilic esophagitis
Apparently “EoE” is a condition only just starting to pick up speed. When I went to the emergency room in 2006, there were very few people in the world that were studying the condition. Even now, most general practitioners aren’t really aware of it and only specialists in gastroenterology are starting to see more patients report symptoms. And before you ask, yes, this affects males more for some reason.
There isn’t any treatment created for this disease, just borrowed methods of managing the causes and outbreaks from other afflictions. For example, I was put on a regimen of one Prilosec a day.
Why a PPI? Well, the reason the strictures occur is a reaction to certain foods. An allergy? Kinda. Sorta. When patients eat certain things (the list is inconclusive at the moment but a pattern is emerging that I’ll talk about later) a specific group of white blood cells (eosinophil) react. Over time doctors noticed that patients taking PPIs saw a reduction in eosinophils.
In my case, upon followup a few months after beginning the PPI regimen, the doctor informed me that they’d basically vanished. A classic case of PPI-responsive eosinophils. He said I was the worst EoE case he’d ever treated, having an enormous number of eosinophils on my initial biopsy. Keep in mind that this wasn’t just any gastroenterologist, he’s a leader in the field with four decades of experience both teaching (USC) and clinical. Since I responded very well to the PPIs, so he recommended taking them “forever.”
Interestingly enough, another emerging treatment for EoE is to spray/swallow topical steroids in the throat. These drugs are already available as OTCs now (Allerflo, etc.). Ironically I’d just seen the ENT a week before about not being able to breathe through my nose at night and he recommended the Allerflo to minimize the polyp and swollen turbinates.
Of course, the biggest change one can make is to eliminate the causes of the white blood cells overproducing in the throat. But this is also the most difficult. So far, doctors have identified a group of likely triggers, which are similar to the list of likely food allergens for sensitive people: milk, wheat, eggs, peanuts, seafood, and Soy.
If you’re starting to guess that multiple health problems might be related to multiple causes without an easy one-size (pill)-fits-all solution you’d be right. And commerce is noticing too. Startups like Everlywell now offer customizable and comprehensive food allergy tests you can take at home. This is a direct result of the negative interactions between people and the food they eat growing, or rather I should say expanding. It used to be that people had common allergies like nuts or lactose; today we’re seeing increasing numbers of people reporting multiple allergic reactions to foods that weren’t considered common allergens in the past. (I was already in that club too, noticing an allergy to avocado when I had a bowl of avocado ice cream in college) And we’re finding out, as I recently did, it may be caused by more than just an allergy.
So, over the past year, I’ve gone on a mission to remove those things from my diet. You can see now that it wasn’t just the barley that caused problems, they just put the white blood cells into over-over-overdrive. All the pizzas and pitas and hamburger buns I’d eaten my entire life had contributed to the strictures as well.
I’d already transitioned away from milk a few years earlier when I noticed an obvious lactose intolerance – but switched to soymilk, which is just as bad for EoE! (at least in theory, it’s unknown whether all six ingredients affect everyone equally) Luckily, coconut milk is becoming as widely available as soy and almond milk.
(I’ve been allergic to nuts my entire life, so almond milk was never going to be an option)
Soy is in everything in small quantities, but I don’t add it in large quantities (soy sauce) so I didn’t have to modify my diet much there. Same story for seafood, lovely when I can get it, but it’s not an everyday item on my plate.
It was wheat that was and is the hardest modification. Almost all bread: gone! Sandwiches: nope! Pizza: How can one live without pizza?!
About a year earlier I’d switched to having a “healthy” veggie wheat wrap for lunch at work every day. Little did I know how unhealthy it was for me. (although to be fair, I knew something in my lunch was causing intestinal distress, but I assumed it was the raw onions or salad dressing)
But, I found an ally to assuage all this dietary stress in hummus.
I used to hate hummus because it was made out of peas, which I’m supposed to be allergic to (and generally don’t like the taste of). But, hummus is made of chickpeas, of course, a different type and flavor of pea. After having hummus included in persian food (which I already liked) I warmed up to it. When it came time to find substitute foods that were nutritious and contained no allergens I started to lean heavily on hummus.
And on vegetables. Although it seems my guts don’t like raw vegetables, I’ve transitioned to a mostly fruit and vegetable diet with a small (fist sized) portion of protein once per day.
You may wonder why I’m focusing so much on changing the input when daily PPIs “fix” the white blood cell build-up.
By four months into the daily PPI regimen, I felt like I had permanent stomach flu. I’d wake up at 4 or 5am and every twenty minutes after that for the next two or three hours. Every day. No matter how much fiber I put in. I’m sure you don’t want to hear more about this, but it’s a very real consequence of long term PPI use just now starting to pick up steam in the medical community.
My doctor recommended I simply switch to another PPI. Hell no! Everything I read indicated that the daily struggle was due to the actual functioning of the PPI, not what brand formula I used. Simply put, lowering stomach acid decreases the ability to digest properly. Decreasing the ability to digest properly also upsets the bacterial balance.
I quit Prilosec cold turkey and began taking probiotics to build back my good flora. After a month or two I was back to normal. During this month I wanted to know if my experience was unique.
I found that using PPIs more than a few weeks is not normal. That’s considered long-term use, and the FDA has released warnings against long term use.
I had taken the damn things daily for months!
Now the stakes are getting even higher for PPIs, with studies reporting increased risk of cancer. In fact, in the few days I was writing this post the FDA released findings of cancer-causing carcinogens in Zantac.
Holy crap! I’ll take some strictures in my throat over, you know, death!
And on that note: It’s been a year and I haven’t experienced an episode. Haven’t had to expel anything. However, I have felt food slow down in there like it used to precipitating a spasm or blockage. After the endoscopic surgery swallowing became automatic and it was a terrific feeling. I’ve had to become cautious again as even with my diet changes the scars seem to be slowly returning. The doctor did warn that this often happens, and folks with this disease have to get their strictures blown out again every few years.
From what I’ve read this condition was unknown to medicine twenty years ago when I first noticed it. Flash forward twenty years and medical studies are being conducted, treatments being evaluated, patients like me improving their lives.
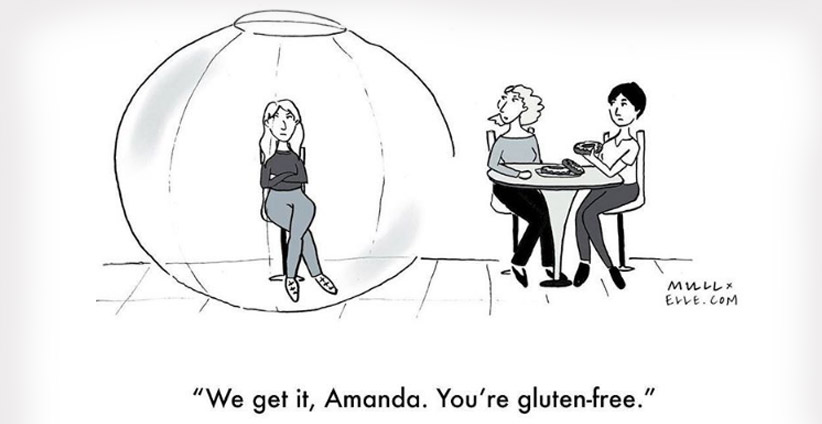
After telling this story to peers and friends it seems in large groups there’s at least one person that knows someone that may be suffering from the same thing. The thinking now is that this is a condition, like autism, that simply went unreported and undiagnosed in the past, but is starting to receive more attention from the medical community. That tends to happen with population growth as the raw number of patients expands by the same ratio and warrants treatment modalities. Combine that with whatever may be “causing” more people to develop food sensitivities and this EoE thing may be the next affliction all the cool kids are pretending to have so they can eat special foods (see ya later Celiac fakers, that’s so last year!).
(to be clear, what my doctor said is that the wheat reaction with EoE is not the same as Celiac’s Disease, it’s a different part of the plant reacting with a different part of the body)
(and even though I just made fun of those gluten-free diet fakers, I’m not one of them since the “gluten-free” label is basically a synonym for wheat-free, which is what I need, so I’ve benefitted from the trend)
I know this is a boring blog post compared to writing about hiking up glaciers in Iceland and swimming with sharks, etc. but I hope that Google spiders this and adds it to the small amount of information about the disease so other folks suffering like I did can find it and know the right questions for their doctor.
If nothing else, when you have to run off to the bathroom you can say “I have an autoimmune disease,” and quiet all those “it’s all in your head” comments!


